Well I have to hand it to my MP, Tom Randall. Whatever it is he wrote in his letter to the hospital it worked. Within days of him writing to them I had been given an appointment with the surgeon at QMC in Nottingham. To be honest I just expected him to say that they still weren’t operating and that it was just a courtesy call on account of my MP having been in touch but that couldn’t have been further from the truth.
I was supposed to have the telephone appointment at 9.40am on Wednesday morning so imagine my surprise when at 9am my phone starts ringing. I was driving Big Girl to school, had the dog in the car cause he was going to doggy daycare and I totally wasn’t expecting it to be Mr E, the surgeon, on the other end of the phone. Luckily I had hands free in the car so I was able to carry on driving and talking, because I wasn’t expecting the conversation to go as it did!
Mr E apologised that he hadn’t been in touch sooner but he had only just received a reply from St Marks. He had written to one of the surgeons there who had operated on me previously to ask her to take a look at my case and to get a second opinion on his surgical plan. I think he was expecting a short, standard response (or hoping that they would offer to take me on as a patient) but what he got was a very detailed letter, laying out a suggested treatment plan. Apparently they had discussed my case in the J-pouch MDT meeting. A MDT meeting is a Multi Disciplinary Team meeting where different medics get together to talk about cases and decide on a treatment plan. In the meeting there were surgeons, gastroenterologists and radiologists and they reviewed all my notes and scans from the last two years.
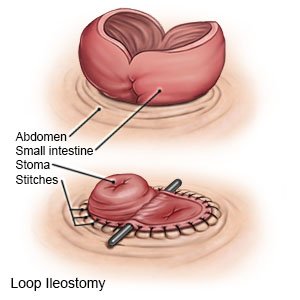
The surgical plan that Mr E had me consent to was basically an ‘open me up and let’s see’ because he doesn’t really know why my bowel is misbehaving so much. There’s the question as to whether I have adhesions or endometriosis (or both, knowing my bloody luck!) wrapped around the bowel or it could be something else entirely. Mr E said that I would more than likely come out of the operation with a loop ileostomy- this is where a loop of small intestine is pulled out through a cut in your abdomen, before being opened up and stitched to the skin to form a stoma.
My gastro consultant in Nottingham has said that there was nothing more that he could do and that surgery was my only option. However, the team at St Marks have suggested three different treatments that I can try with surgery being a very last resort. So what are these treatments?? Here goes…
1) They’re going to treat me for SIBO (Small intestine bacterial overgrowth) This is where there is an increase in the bacteria population in your small intestine; normally it cannot survive there because of stomach acid and other body fluids but one of the causes of SIBO is bowel obstructions and we all know I’ve had a few of those in the last year or so! So I will need to go on a prolonged course of antibiotics to try and get this under control. Of course I’m allergic to the first choice antibiotic so they’re looking into what they can prescribe, at what dose and for how long as St Marks and Nottingham have differing guidelines.
2) I’m going to go on a high dose steroid treatment. When I was on steroids previously they did help, but only at the very high doses. So the plan is put me on a high dose again but with a different type of steroid. I was on prednisolone previously but this new one begins with a R, I think. Because I was driving I couldn’t take notes and my memory is bloody awful but it will all be in the letter that Mr E dictates summarising our conversation so I’m not too worried.
3) The surgical Prof at St Marks has suggested that I then go on a biological treatment. This is because the question mark of whether I have Crohn’s disease still seems to be hanging over me. Every couple of years they seem to revisit this question and generally decide that I don’t, but maybe I could have. But because they don’t see crohns when they do the endoscopies they don’t treat me for it. However, the Prof thinks I probably do have it but in the deeper layers of my bowel which is why it’s never shown up on the scopes. When I was an inpatient last summer and at my absolute wits end I did persuade Dr B, my gastro consultant, to give me a dose of a biological treatment in the hope that it might help. But because I didn’t see any changes after 1 treatment he refused to prescribe more, despite best practice saying that a minimum of 3 treatments are needed. At the time I was just so, so poorly I didn’t have the fight in me, but now I do.
Apparently Mr E spoke to Dr B before calling me to go through these suggested treatments but he wasn’t on board with them. According to Mr E, Dr B is very old school and just hasn’t kept up to date with the use of biological treatments for IBD. He doesn’t agree with them and generally doesn’t prescribe them despite the evidence for them being overwhelming. Lots of patients report having their IBD put into remission by the right biological treatment and I’m hopeful it could go the same for me. So Dr B has stepped back from my gastro care and the new gastr consultant at the hospital, Dr P, will take over. Dr P did his fellowship at St Marks so he already has a big tick from me ✅ He is more IBD focused whereas Dr B tends to focus on the nutrition side of bowel disease and looks after TPN patients. So I’m really optimistic that between the two of them I will get really well rounded care. The only downside is that I have to wait for Mr E to contact Dr P and then I have to be seen in one of his clinics so I’m not sure when I will be able to begin with the plan.
4) Surgery. This still stays on the table but as I said before, as a last resort. The St Marks Prof isn’t hopeful that surgery will be the answer that I’m looking for and isn’t confident that I will have a good surgical outcome. She has revised Mr E’s surgical plan and has suggested that instead of a loop ileostomy he performs an end ileostomy. This would mean they would cut through my small intestine leaving the J-pouch in situ but defunctioned.
Having an end ileostomy makes further surgery to join me back up much, much more difficult but it does mean that they can remove a section of my small bowel and send it away to the lab for tests. This would hopefully answer the question of whether I have crohns or an other problem within the bowel. But leaving a defunctioned J-pouch carries risk and about 50% of people who have this operation then go on to need further surgery to remove the J-pouch because they have ongoing issues and infections. Removing a J-pouch is a HUGE operation and not one that I would fancy doing. It would also leave me with what’s known within the bowel disease community as the ‘Barbie Bum’. That’s where you have your anus sown up so nothing can come out of it any more (just like a Barbie doll’s!) This surgery has a high rate of infection and post op complications and recovery is long and slow so I would prefer to avoid this if at all possible.
The other thing that concerned the Prof was that my two previous stomas caused me so many problems. The first one used to block and not work properly which is what lead me to have the J-pouch surgery in the first place. And then the temporary stoma I had for 6 months in between the two J-pouch surgeries was really high output. It was awful- poo just poured and poured out and getting a stoma bag to stay on was almost impossible. It also caused terrible dehydration and that was when I first had a Hickman line to have IV fluids because any fluids I drank passed straight through me and took all the electrolytes with it making me really poorly. So the thought that I could end up with a stoma like this again terrifies me. And this time it would be for longer than 6 months. I really don’t know if I could cope with a stoma like that. Although it might stop the obstructions from happening it would create a whole host of new problems.
So Mr E asked me what I wanted to do. Did I want to try the treatments suggested by the Prof at St Marks or did I just want to wait for surgery? I told him it would be remiss of me to ignore the advice of one of the UK’s (if not the world’s) leading bowel surgeons who has probably treated more people like me than she’s had hot dinners. Although in Nottingham I’m their most complicated case and a complete nightmare, to St Marks I’m just another patient and probably one of their easier ones to be honest! And given the fact that I could be waiting 6, 10, 12 months or more for any surgery I think it would be crazy not to try these things while I’m waiting. Mr E said he will leave me on the waiting list so if these treatments fail then I’m not having to join the bottom of the waiting list again and hopefully by that time he will be allowed to be operating on more than just cancer and life threatening bowel disease cases.
I had become so exasperated waiting for a surgery date that I had booked an appointment to see a private surgeon to explore my options. Although I’m pretty sure I couldn’t be operated on privately on account of needing a HDU/ITU bed afterwards I wanted to know for sure. I also wanted to get an idea of the cost if it were possible. But given the conversation I had with Mr E yesterday I decided to cancel that appointment. Like Hubby said, a private surgeon will want to cut. He’s getting paid big bucks to tell me that he could do the surgery and that what he could do would make me better and possibly be a miracle cure. And whilst I like to think that I’m not gullible enough to fall for that there is a slim chance that his patter could be smooth enough to get me handing over my credit card and opening my diary!
So although there’s no surgery date I feel hopeful for the first time in the last couple of years. The last few months I’ve felt like I’ve been living in limbo and whilst and I’ve been fairly well and I’ve not been in hospital this year it’s felt like having the sword of Damocles hanging over me. Do I think that one of these treatments will work? Past experience tells me to assume the worst and think no. In the 14 years I’ve lived with bowel disease all the conventional treatments have failed, my surgeries have had complications and when they’ve told me there’s a 1% chance of something happening I’ve been that 1%. But part of me dares to dream. What if one, or a combination of all of these treatments, work and give me back some kind of quality of life? I’ve spent my late 20’s and almost of my 30’s being sick and having to make all of my life decisions based on my illness. What if I do go into remission and for the first time for a long time I am well? Would I even know how to live life not being poorly? Probably not but I reckon I could learn!!

Comments
Post a Comment